Authors

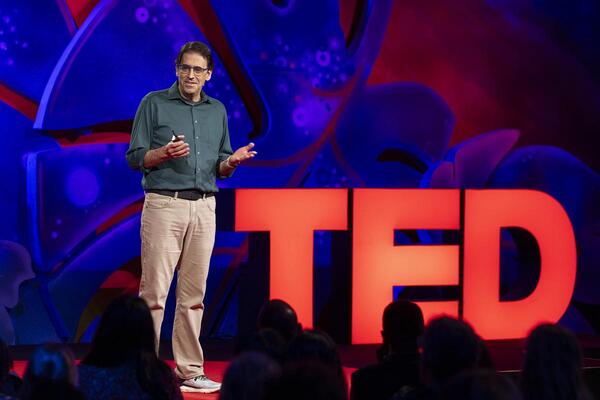
Dr. Akhila Kosaraju is the CEO and President of Phare Bio, a social venture pioneering the use of generative AI and deep learning to discover new classes of antibiotics, in collaboration with the Collins Lab at MIT. Under her leadership, Phare Bio launched with funding and support from TED’s Audacious Project, which backs bold solutions to the world’s most urgent challenges. The company has since been awarded $27 million from the Advanced Research Projects Agency for Health (ARPA-H), selected for Google.org’s Generative AI Accelerator, and named to Fast Company’s 2025 World Changing Ideas list. Phare has also received a Newsweek AI Impact Award and was chosen as Wired Health’s Startup Showcase Winner.
Dr. Kosaraju has spent her career building companies and driving innovation at the intersection of infectious disease and computational biology. She was the founding CEO of Variant Bio, a venture-backed genomics and therapeutics company, and previously served as an executive at SIGA Technologies, where she helped bring antiviral drugs to market. During her tenure at SIGA, the company secured FDA approval for a novel smallpox antiviral and partnered with the CDC, BARDA, and DoD to deliver 2 million treatment courses to the U.S. Strategic National Stockpile.
Earlier in her career, Dr. Kosaraju was a White House appointee at the Pentagon, where she served as Special Assistant to the Assistant Secretary of Defense for Health Affairs. There, she provided executive leadership for the $50 billion Military Health System, overseeing military healthcare delivery, biodefense, and international humanitarian programs.
She is a recipient of the Office of the Secretary of Defense Medal for Exceptional Public Service, the highest non-career civilian honor within the Department of Defense. Dr. Kosaraju is a Member of the Council on Foreign Relations, co-founder of the Alliance to End Biological Threats, and a Lecturer at Stanford’s Center for Biosecurity and Pandemic Resilience. She earned her M.D. from Columbia University’s College of Physicians and Surgeons and holds a B.A. in Human Biology from Stanford University.
Categories
Subscribe for updates
September 5, 2025
The Hill
We need more open science in biotech — here’s how we achieve it
In the “Golden Age” of antibiotic discovery during the 1950s and ’60s, pharmaceutical companies, research institutions and scientists joined forces in a global hunt for life-saving compounds. They scoured soil samples from the Amazon to the Himalayas, exchanged microbial strains across institutions, and shared discoveries — like Streptomycin, the first effective treatment for tuberculosis — within weeks, a previously unprecedented pace. It was a time when science advanced rapidly through remarkable openness and collaboration.
In the decades since, antibiotic resistance has grown into a full-blown crisis — not for lack of scientific know-how or effort, but because of deeper structural challenges. Still, the collaborative spirit of that era offers a powerful model for how we can respond.
According to the World Health Organization, antimicrobial resistance is one of the top 10 global public health threats facing humanity, yet only a handful of new antibiotics have been approved in recent years. With limited financial upside, small, mission-driven teams are now carrying the torch for antibiotic discovery — working with a fraction of the resources and an ever-growing demand for high-quality data. Today, just three major pharmaceutical companies continue to maintain antibiotic discovery programs, as the vast majority have exited the field.
Most new antibiotics earn less than $50 million per year, despite treating millions. Meanwhile, other areas of medicine can generate billions annually, often while serving smaller patient populations. This disparity highlights how market incentives don’t always align with urgent public health needs.
Already, antibiotic resistance is responsible for over 1.27 million deaths annually — contributing to nearly 5 million deaths in total — and without intervention, it risks becoming one of the leading causes of death worldwide by 2050.




.jpg)